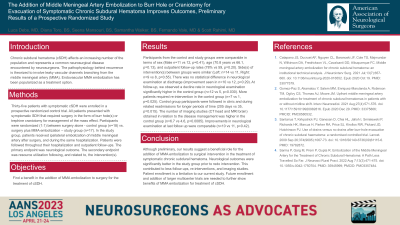
The Addition of Middle Meningeal Artery Embolization to Craniotomy for Evacuation of Symptomatic Chronic Subdural Hematoma Improves Outcomes, Preliminary Results of a Prospective Randomized Study
Friday, April 21, 2023

Luca H. Debs, MD
Resident
Medical College of Georgia
Augusta, Georgia, United States
ePoster Presenter(s)
Introduction: Standard management of symptomatic chronic subdural hematoma (cSDH) typically involves surgical evacuation. Reported rates of recurrence following intervention are up to 39%. The pathophysiology behind recurrence is theorized to involve leaky vascular channels branching from the middle meningeal artery (MMA). Endovascular MMA embolization has been popularized as a treatment option. Well-designed studies have shown a role in its application, but further investigation is warranted. Here, we present the first randomized controlled prospective study aimed at comparing embolization following surgery to surgery alone.
Methods: Twenty-nine patients with symptomatic cSDH requiring surgery for management of mass effect were enrolled in a prospective randomized control trial. After consent was obtained all participants were randomized (1:1) between surgery alone - control group (n=15) vs. surgery plus MMA embolization – study group (n=14). In the study group, patients received ipsilateral embolization of middle meningeal artery after surgery. The primary endpoint was neurological outcome. The secondary endpoint was resource utilization following, and related to, the intervention(s).
Results: Participants from the control and study groups were comparable in terms of sex, age, follow-up rates and neurological examination at discharge. At follow-up, we observed a decline rate in neurological examination significantly higher in the control group (n=10 vs 3, p=0.031). Further, control group patients required more re-interventions (n=7 vs 1, p=0.022), were followed for longer periods of time (238 days vs 37, p=0.016), and had a higher number of imaging studies obtained (n=7.3 vs 5, p= 0.0074).
Conclusion : Our results suggest a beneficial role for the addition of MMA embolization to surgical intervention in the treatment of symptomatic chronic subdural hematoma. Neurological outcomes were significantly better in the study group. This contributed to less follow-ups, re-interventions, and imaging studies. Future enrollment and addition of larger multicenter trials are needed to further show benefits of MMA embolization for treatment of cSDH.
Methods: Twenty-nine patients with symptomatic cSDH requiring surgery for management of mass effect were enrolled in a prospective randomized control trial. After consent was obtained all participants were randomized (1:1) between surgery alone - control group (n=15) vs. surgery plus MMA embolization – study group (n=14). In the study group, patients received ipsilateral embolization of middle meningeal artery after surgery. The primary endpoint was neurological outcome. The secondary endpoint was resource utilization following, and related to, the intervention(s).
Results: Participants from the control and study groups were comparable in terms of sex, age, follow-up rates and neurological examination at discharge. At follow-up, we observed a decline rate in neurological examination significantly higher in the control group (n=10 vs 3, p=0.031). Further, control group patients required more re-interventions (n=7 vs 1, p=0.022), were followed for longer periods of time (238 days vs 37, p=0.016), and had a higher number of imaging studies obtained (n=7.3 vs 5, p= 0.0074).
Conclusion : Our results suggest a beneficial role for the addition of MMA embolization to surgical intervention in the treatment of symptomatic chronic subdural hematoma. Neurological outcomes were significantly better in the study group. This contributed to less follow-ups, re-interventions, and imaging studies. Future enrollment and addition of larger multicenter trials are needed to further show benefits of MMA embolization for treatment of cSDH.
