The Socioeconomic Distressed Communities Index (DCI) Predicts 90-day Mortality among Brain Tumor Patients
The Socioeconomic Distressed Communities Index (DCI) Predicts 90-day Mortalityamong Brain Tumor Patients
Friday, April 21, 2023

Debraj Mukherjee, MD, MPH (he/him/his)
Assistant Professor
Johns Hopkins University School of Medicine
Baltimore, MD, US
ePoster Presenter(s)
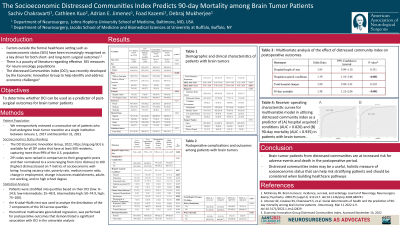
Introduction: Socioeconomic status (SES) is a major determinant of quality of life, healthcare-related outcomes, and mortality. However, it remains difficult to comprehensively measure SES on a large scale. The distress communities index (DCI), a composite of seven social determinants of health factors, has been increasingly recognized for its correlation with poor outcomes. We sought to determine the predictive value of DCI on complications and outcomes following brain tumor surgery.
Methods: A single institution, retrospective chart review was conducted to identify adult brain tumor patients undergoing resection (2017–2021). Patient ZIP codes were matched to DCI, which accounts for unemployment, education, poverty, median income, business growth, and housing vacancies, and stratified by DCI quartiles (low: 0–24.9, low-intermediate: 25–49.9, intermediate-high: 50–74.9, high: 75–100). Univariate followed by multivariate regressions assessed the effects of DCI on postoperative outcomes. Receiver operating curves (ROCs) were generated for prediction of significant outcomes.
Results: A total of 2,389 patients (mean age, 55.47±15.00 years; male, 47.0%) were included: 1015 patients (42.5%) resided in low distress communities, 689 (28.8%) in low-intermediate distress communities, 445 (18.6%) in intermediate-high distress communities, and 240 (10.0%) in high distress communities. On multivariate analysis, risk of hospital-acquired conditions (HAC) (adjusted odds ratio [aOR]=1.39, 95% confidence interval [CI] 1.18–1.66, p< 0.001) and 90-day mortality (aOR=1.58, 95%CI 1.21–2.06, p< 0.001) increased with increasing DCI quartile. Good predictive accuracy was observed for both models, with ROC of 0.826 (95%CI 0.780–0.872) for HAC and 0.935 (95%CI 0.906–0.973) for 90-day mortality.
Conclusion : Brain tumor patients from distressed communities are at an increased risk for adverse events and death in the postoperative period. DCI may be a useful, holistic measure of socioeconomic status that can help risk stratifying patients and should be considered when building healthcare pathways.
Methods: A single institution, retrospective chart review was conducted to identify adult brain tumor patients undergoing resection (2017–2021). Patient ZIP codes were matched to DCI, which accounts for unemployment, education, poverty, median income, business growth, and housing vacancies, and stratified by DCI quartiles (low: 0–24.9, low-intermediate: 25–49.9, intermediate-high: 50–74.9, high: 75–100). Univariate followed by multivariate regressions assessed the effects of DCI on postoperative outcomes. Receiver operating curves (ROCs) were generated for prediction of significant outcomes.
Results: A total of 2,389 patients (mean age, 55.47±15.00 years; male, 47.0%) were included: 1015 patients (42.5%) resided in low distress communities, 689 (28.8%) in low-intermediate distress communities, 445 (18.6%) in intermediate-high distress communities, and 240 (10.0%) in high distress communities. On multivariate analysis, risk of hospital-acquired conditions (HAC) (adjusted odds ratio [aOR]=1.39, 95% confidence interval [CI] 1.18–1.66, p< 0.001) and 90-day mortality (aOR=1.58, 95%CI 1.21–2.06, p< 0.001) increased with increasing DCI quartile. Good predictive accuracy was observed for both models, with ROC of 0.826 (95%CI 0.780–0.872) for HAC and 0.935 (95%CI 0.906–0.973) for 90-day mortality.
Conclusion : Brain tumor patients from distressed communities are at an increased risk for adverse events and death in the postoperative period. DCI may be a useful, holistic measure of socioeconomic status that can help risk stratifying patients and should be considered when building healthcare pathways.
