90-day Readmission after Subdural Hematoma
90-day Readmission After Subdural Hematoma
Friday, April 21, 2023

Suzanne Gross
Medical Student
Albert Einstein College of Medicine
Miami Beach, Florida, United States
ePoster Presenter(s)
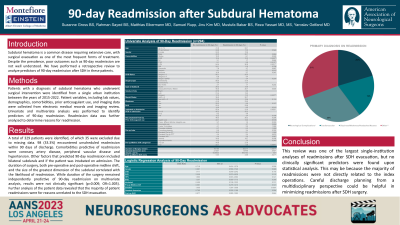
Introduction: Subdural hematoma is a common disease requiring extensive care, with surgical evacuation as one of the most frequent forms of treatment. Despite the prevalence, poor outcomes such as 90-day readmission are not well understood. We have performed a retrospective review to analyze predictors of 90-day readmission after SDH in these patients.
Methods: Patients with a diagnosis of subdural hematoma who underwent surgical intervention were identified from a single urban institution between the years of 2015-2022. Patient variables, including lab values, demographics, comorbidities, prior anticoagulant use, and imaging data were collected from electronic medical records and imaging review. Univariate and multivariate analysis was performed to identify predictors of 90-day readmission. Readmission data was further analyzed to determine reasons for readmission.
Results: A total of 329 patients were identified, of which 35 were excluded due to missing data. 98 (33.3%) encountered unscheduled readmission within 90 days of discharge. Comorbidities predictive of readmission were coronary artery disease, peripheral vascular disease and hypertension. Other factors that predicted 90-day readmission included bilateral subdurals and if the patient was intubated on admission. The duration of surgery, both pre-operative and post-operative midline shift, and the size of the greatest dimension of the subdural correlated with the likelihood of readmission. While duration of the surgery remained independently predictive of 90-day readmission on multivariate analysis, results were not clinically significant (p=0.009, OR=1.005). Further analysis of the patient data revealed that the majority of patient readmissions were for reasons unrelated to the SDH evacuation.
Conclusion : This review was one of the largest single-institution analyses of readmissions after SDH evacuation, but no clinically significant predictors were found upon statistical analysis. This may be because the majority of readmissions were not directly related to the index operations. Careful discharge planning from a multidisciplinary perspective could be helpful in minimizing readmissions after SDH surgery.
Methods: Patients with a diagnosis of subdural hematoma who underwent surgical intervention were identified from a single urban institution between the years of 2015-2022. Patient variables, including lab values, demographics, comorbidities, prior anticoagulant use, and imaging data were collected from electronic medical records and imaging review. Univariate and multivariate analysis was performed to identify predictors of 90-day readmission. Readmission data was further analyzed to determine reasons for readmission.
Results: A total of 329 patients were identified, of which 35 were excluded due to missing data. 98 (33.3%) encountered unscheduled readmission within 90 days of discharge. Comorbidities predictive of readmission were coronary artery disease, peripheral vascular disease and hypertension. Other factors that predicted 90-day readmission included bilateral subdurals and if the patient was intubated on admission. The duration of surgery, both pre-operative and post-operative midline shift, and the size of the greatest dimension of the subdural correlated with the likelihood of readmission. While duration of the surgery remained independently predictive of 90-day readmission on multivariate analysis, results were not clinically significant (p=0.009, OR=1.005). Further analysis of the patient data revealed that the majority of patient readmissions were for reasons unrelated to the SDH evacuation.
Conclusion : This review was one of the largest single-institution analyses of readmissions after SDH evacuation, but no clinically significant predictors were found upon statistical analysis. This may be because the majority of readmissions were not directly related to the index operations. Careful discharge planning from a multidisciplinary perspective could be helpful in minimizing readmissions after SDH surgery.
