Disparities in adult primary spinal malignancy survival by Medicaid-status: A nationwide analysis
Disparities in Adult Primary Spinal Malignancy Survival by Medicaid-status: A Nationwide Analysis
Friday, April 21, 2023

Arjun Ganga, BS
Medical student (M3)
Warren Alpert Medical School of Brown University
ePoster Presenter(s)
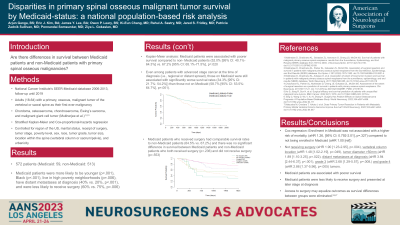
Introduction: The relationship between survival outcomes of patients with spinal primary malignant bone tumors (sPMBT) and health insurance status is understudied, though the important relationship between these variables has been demonstrated in other healthcare contexts.
Methods: Using the newly created SEER-Medicaid database, adults diagnosed between 2006-2013 with sPMBT including chordoma, osteosarcoma, chondrosarcoma, Ewing’s sarcoma, or malignant giant cell tumor (GCT) were studied. Five-year survival analysis was performed using the Kaplan-Meier method. Adjusted survival analysis was performed using Cox proportional hazards regression controlling for age, sex, marital status, cancer stage, poverty level, vertebral versus sacral location, geography, rurality, tumor diameter, tumor grade, tumor histology, and therapy including surgery, radiation, and chemotherapy.
Results: 572 patients with sPMBT (n=59 on Medicaid) were identified. There were significantly more patients with GCT (6.8% vs. 1.2%, p=.002) and osteosarcoma (28.8% vs. 17.3%, p=.032) in the Medicaid group with no other significant differences regarding pathology. Medicaid patients were more likely to be younger (p < .001), Black (p < .001), live in high poverty neighborhoods (p=.006), have distant metastases at diagnosis (p < .001), and less likely to receive surgery (p=.006). The 5-year survival rate was 65.7% (Chondrosarcoma: 70.0%, Chordoma: 91.5%, Ewing’s Sarcoma: 44.6%, GCT: 90.0%, Osteosarcoma: 34.2%). Medicaid patients had significantly worse 5-year survival than non-Medicaid patients (52.0% vs. 67.2%, p=.02). Minorities on Medicaid were associated with an increased risk of cancer-specific mortality compared to White non-Medicaid patients (aHR=2.51, 95% CI: 1.18-5.35, p=.017). Among Medicaid patients, those who received surgery had significantly better survival than those who did not (64.5% vs. 30.6%, p=.001). For all patients, not receiving surgery (aHR=1.90 [1.23-2.95], p=.004) and tumor diameter >50mm (aHR=1.89 [1.10-3.25], p=.023) were independently associated with an increased risk of mortality.
Conclusion : Medicaid patients may be less likely to receive surgery and suffer from poorer 5-year, cancer-specific survival than non-Medicaid patients. These disparities may be especially prominent among minorities.
Methods: Using the newly created SEER-Medicaid database, adults diagnosed between 2006-2013 with sPMBT including chordoma, osteosarcoma, chondrosarcoma, Ewing’s sarcoma, or malignant giant cell tumor (GCT) were studied. Five-year survival analysis was performed using the Kaplan-Meier method. Adjusted survival analysis was performed using Cox proportional hazards regression controlling for age, sex, marital status, cancer stage, poverty level, vertebral versus sacral location, geography, rurality, tumor diameter, tumor grade, tumor histology, and therapy including surgery, radiation, and chemotherapy.
Results: 572 patients with sPMBT (n=59 on Medicaid) were identified. There were significantly more patients with GCT (6.8% vs. 1.2%, p=.002) and osteosarcoma (28.8% vs. 17.3%, p=.032) in the Medicaid group with no other significant differences regarding pathology. Medicaid patients were more likely to be younger (p < .001), Black (p < .001), live in high poverty neighborhoods (p=.006), have distant metastases at diagnosis (p < .001), and less likely to receive surgery (p=.006). The 5-year survival rate was 65.7% (Chondrosarcoma: 70.0%, Chordoma: 91.5%, Ewing’s Sarcoma: 44.6%, GCT: 90.0%, Osteosarcoma: 34.2%). Medicaid patients had significantly worse 5-year survival than non-Medicaid patients (52.0% vs. 67.2%, p=.02). Minorities on Medicaid were associated with an increased risk of cancer-specific mortality compared to White non-Medicaid patients (aHR=2.51, 95% CI: 1.18-5.35, p=.017). Among Medicaid patients, those who received surgery had significantly better survival than those who did not (64.5% vs. 30.6%, p=.001). For all patients, not receiving surgery (aHR=1.90 [1.23-2.95], p=.004) and tumor diameter >50mm (aHR=1.89 [1.10-3.25], p=.023) were independently associated with an increased risk of mortality.
Conclusion : Medicaid patients may be less likely to receive surgery and suffer from poorer 5-year, cancer-specific survival than non-Medicaid patients. These disparities may be especially prominent among minorities.
