Student-Led Neurosurgical Simulation for Team-Building in Medical Instruction
Student-led Neurosurgical Simulation for Team-building in Medical Instruction
Friday, April 21, 2023

Alex Gilman, BS (he/him/his)
Medical Student
Boonshoft School of Medicine at Wright State University
Dayton, Ohio, United States
ePoster Presenter(s)
Introduction: We hypothesized that medical students would develop skills in critical thinking, multidisciplinary communication, professionalism, and leadership during role-played simulations of complex care. Here we present a student-led neurosurgical simulation that drew a high level of interest and participation among medical students at our institution, leading to improved engagement during anatomy, physiology, and pathology instruction.
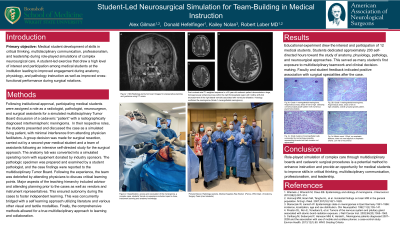
Methods: Following institutional approval, participating medical students were assigned a role as a radiologist, pathologist, neurosurgeon, and surgical assistants for a simulated multidisciplinary Tumor Board discussion of a cadaveric “patient” with a radiographically diagnosed interhemispheric meningioma. In their respective roles, the students presented and discussed the case as a simulated living patient, with minimal interference from attending physician facilitators. A group decision was made for surgical resection, carried out by a second-year medical student and a team of assistants following an intensive self-directed study for the surgical approach. The anatomy lab was converted into a simulated operating room with equipment donated by industry sponsors. The pathologic specimen was prepared and examined by a student pathologist, and the case findings were reported to the multidisciplinary Tumor Board. Following the experience, the team was debriefed by attending physicians to discuss critical learning points.
Results: This educational experiment drew the interest and participation of twelve students, who dedicated approximately two hundred self-directed hours toward the study of anatomy, physiology, pathology, and neurosurgical approaches. For many students, this simulation was the first exposure to multidisciplinary teamwork and clinical decision-making and was an essential team-building exercise. The program received excellent feedback from a survey of the participants.
Conclusion : Role-played simulation of complex care through multidisciplinary boards and cadaveric surgical procedures is a potential method to enhance instruction and provide an opportunity for medical students to improve skills in critical thinking, multidisciplinary communication, professionalism, and leadership.
Methods: Following institutional approval, participating medical students were assigned a role as a radiologist, pathologist, neurosurgeon, and surgical assistants for a simulated multidisciplinary Tumor Board discussion of a cadaveric “patient” with a radiographically diagnosed interhemispheric meningioma. In their respective roles, the students presented and discussed the case as a simulated living patient, with minimal interference from attending physician facilitators. A group decision was made for surgical resection, carried out by a second-year medical student and a team of assistants following an intensive self-directed study for the surgical approach. The anatomy lab was converted into a simulated operating room with equipment donated by industry sponsors. The pathologic specimen was prepared and examined by a student pathologist, and the case findings were reported to the multidisciplinary Tumor Board. Following the experience, the team was debriefed by attending physicians to discuss critical learning points.
Results: This educational experiment drew the interest and participation of twelve students, who dedicated approximately two hundred self-directed hours toward the study of anatomy, physiology, pathology, and neurosurgical approaches. For many students, this simulation was the first exposure to multidisciplinary teamwork and clinical decision-making and was an essential team-building exercise. The program received excellent feedback from a survey of the participants.
Conclusion : Role-played simulation of complex care through multidisciplinary boards and cadaveric surgical procedures is a potential method to enhance instruction and provide an opportunity for medical students to improve skills in critical thinking, multidisciplinary communication, professionalism, and leadership.
