Smartphone Pupillometry in Acute Mild Traumatic Brain Injury: A Pilot Study
Friday, April 21, 2023

Anthony J. Maxin, BS (he/him/his)
Medical Student
University of Washington Department of Neurological Surgery; Creighton University School of Medicine
Omaha, Nebraska, United States
ePoster Presenter(s)
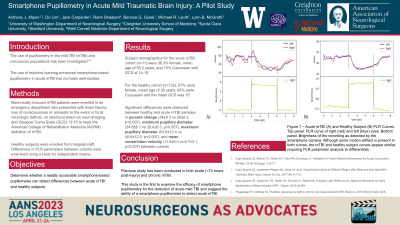
Introduction: The pupillary light reflex (PLR) is a biomarker of neurological disease that is used in the management of moderate to severe traumatic brain injury (TBI). While the use of pupillometry in the mild TBI (mTBI) and concussion populations has been investigated, the use of machine learning-enhanced smartphone-based pupillometry in acute mTBI has not been well-studied. We present pilot data comparing PLR parameters (maximum and minimum diameter, percent change in diameter, latency of light response, mean and maximum constriction velocity, and dilation velocity) in a cohort of acute mTBI patients compared to healthy controls.
Methods: Mild TBI patients were enrolled in an emergency department who presented with head trauma, loss of consciousness or amnestic to the event or focal neurologic deficits, no structural lesion on neuroimaging, and Glasgow Coma Scale (GCS) 13-15 to meet the American College of Rehabilitation Medicine (ACRM) definition of mTBI. Healthy subjects were enrolled from hospital staff. Differences in PLR parameters between cohorts were examined using a t-test for independent means.
Results: A total of n=11 patients with diagnosed acute mild TBI and n=132 healthy subjects were enrolled. Subject demographics were 50% female, mean age 65, 10 Caucasian, 1 African American in the mTBI cohort and 67% female, mean age 36, 84 Caucasian, 12 African American, 24 Asian, 8 Hispanic, 4 Native American in the healthy cohort. Mean GCS was 14.9. Subjects with abnormal head CT scans were excluded. All subjects met the ACRM criteria. Significant (p < 0.05) differences were observed in PLR parameters of maximum diameter, % change, mean constriction velocity, and mean dilation velocity.
Conclusion : We demonstrate the capability of a smartphone-based pupillometer to discern mTBI in an acute setting. Further study in the acute mTBI population is indicated.
Methods: Mild TBI patients were enrolled in an emergency department who presented with head trauma, loss of consciousness or amnestic to the event or focal neurologic deficits, no structural lesion on neuroimaging, and Glasgow Coma Scale (GCS) 13-15 to meet the American College of Rehabilitation Medicine (ACRM) definition of mTBI. Healthy subjects were enrolled from hospital staff. Differences in PLR parameters between cohorts were examined using a t-test for independent means.
Results: A total of n=11 patients with diagnosed acute mild TBI and n=132 healthy subjects were enrolled. Subject demographics were 50% female, mean age 65, 10 Caucasian, 1 African American in the mTBI cohort and 67% female, mean age 36, 84 Caucasian, 12 African American, 24 Asian, 8 Hispanic, 4 Native American in the healthy cohort. Mean GCS was 14.9. Subjects with abnormal head CT scans were excluded. All subjects met the ACRM criteria. Significant (p < 0.05) differences were observed in PLR parameters of maximum diameter, % change, mean constriction velocity, and mean dilation velocity.
Conclusion : We demonstrate the capability of a smartphone-based pupillometer to discern mTBI in an acute setting. Further study in the acute mTBI population is indicated.
