Early Neuroworsening Predicts Traumatic Brain Injury Severity and Outcome
Friday, April 21, 2023

John K. Yue, MD
Neurosurgery Resident (PGY-5)
University of California San Francisco
Daly City, California, United States
ePoster Presenter(s)
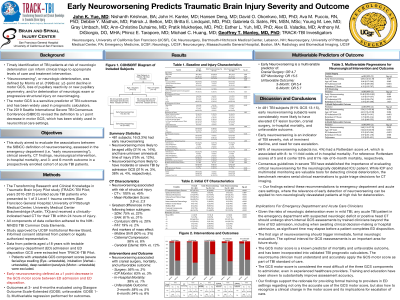
Introduction: Neuroworsening is considered a symptom of progressive brain damage and herald of deterioration. Its utility as an endpoint for traumatic brain injury (TBI) clinical trials requires further validation.
Methods: Adult TBI patients from the prospective, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury Pilot Study with testable emergency department (ED) admission and discharge Glasgow Coma Scale (GCS) scores were extracted. Early neuroworsening was defined as lower motor GCS at ED discharge compared to ED admission. Clinical characteristics, intracranial injury on computed tomography (CT), procedural intervention, in-hospital mortality, and 3- and 6-month outcome (Glasgow Outcome Scale-Extended; GOSE) were evaluated across patients with vs. without neuroworsening.
Results: In 481 patients, 16 (3.3%) had early neuroworsening. Patients with neuroworsening were more likely to be aged ≥65 (31.3%/13.5%; p=0.046), have moderate (31.3%/2.6%) or severe TBI (37.5%/4.3%), unknown posttraumatic amnesia (73.3%/11.4%), require mannitol in ED (12.5%/0.9%) and intensive care unit admission (100%/26.2%; all p< 0.001). Patients with neuroworsening were 100% CT-positive (vs. 45.4%), with increased incidence of subdural hematoma (75.0%/22.2%), subarachnoid hemorrhage (81.3%/31.2%), contusion (68.8%/20.4%), intraventricular hemorrhage (18.8%/2.2%), midline shift (50%/2.6%), cisternal compression (56.3%/5.6%), and brain swelling (68.8%/12.3%; all p< 0.001). Neuroworsening was associated with increased cranial surgery (56.3%/3.5%), intracranial monitoring (62.5%/2.6%), in-hospital mortality (37.5%/0.6%; p< 0.001), and unfavorable outcome (GOSE 1-4; 3-month: 75.0%/8.5%; 6-month: 61.5%/8.4%; p< 0.001). No significant between-group differences were observed for sex, loss of consciousness, intoxication, or polytrauma. When stratified by TBI severity (GCS 3-12 vs. 13-15), differences in age, mortality and unfavorable outcome were driven by patients with moderate/severe TBI, while other differences were conserved across severities.
Conclusion : Early neuroworsening in the ED is a marker of increased clinical and radiographic TBI severity, treatment intensity, in-hospital mortality, and 3- and 6-month unfavorable outcome. Patients with early neuroworsening require early detection and treatment to limit injury evolution and improve prognosis.
Methods: Adult TBI patients from the prospective, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury Pilot Study with testable emergency department (ED) admission and discharge Glasgow Coma Scale (GCS) scores were extracted. Early neuroworsening was defined as lower motor GCS at ED discharge compared to ED admission. Clinical characteristics, intracranial injury on computed tomography (CT), procedural intervention, in-hospital mortality, and 3- and 6-month outcome (Glasgow Outcome Scale-Extended; GOSE) were evaluated across patients with vs. without neuroworsening.
Results: In 481 patients, 16 (3.3%) had early neuroworsening. Patients with neuroworsening were more likely to be aged ≥65 (31.3%/13.5%; p=0.046), have moderate (31.3%/2.6%) or severe TBI (37.5%/4.3%), unknown posttraumatic amnesia (73.3%/11.4%), require mannitol in ED (12.5%/0.9%) and intensive care unit admission (100%/26.2%; all p< 0.001). Patients with neuroworsening were 100% CT-positive (vs. 45.4%), with increased incidence of subdural hematoma (75.0%/22.2%), subarachnoid hemorrhage (81.3%/31.2%), contusion (68.8%/20.4%), intraventricular hemorrhage (18.8%/2.2%), midline shift (50%/2.6%), cisternal compression (56.3%/5.6%), and brain swelling (68.8%/12.3%; all p< 0.001). Neuroworsening was associated with increased cranial surgery (56.3%/3.5%), intracranial monitoring (62.5%/2.6%), in-hospital mortality (37.5%/0.6%; p< 0.001), and unfavorable outcome (GOSE 1-4; 3-month: 75.0%/8.5%; 6-month: 61.5%/8.4%; p< 0.001). No significant between-group differences were observed for sex, loss of consciousness, intoxication, or polytrauma. When stratified by TBI severity (GCS 3-12 vs. 13-15), differences in age, mortality and unfavorable outcome were driven by patients with moderate/severe TBI, while other differences were conserved across severities.
Conclusion : Early neuroworsening in the ED is a marker of increased clinical and radiographic TBI severity, treatment intensity, in-hospital mortality, and 3- and 6-month unfavorable outcome. Patients with early neuroworsening require early detection and treatment to limit injury evolution and improve prognosis.
