Using Machine Learning to Identify Patients Likely To Choose Surgery For One Level Anterior Cervical Disc Herniations
Using Machine Learning to Identify Patients Likely to Choose Surgery for One Level Anterior Cervical Disc Herniations
Friday, April 21, 2023

John Stokes, MD
Neurosurgeon
Ascension Texas Spine and Scoliosis
Austin, Texas, United States
ePoster Presenter(s)
Introduction: This study aims to investigate if machine learning can identify factors associated with the likelihood of a patient will ultimately choose surgical intervention for one level cervical disc herniation?
Methods: 130 retrospective chart reviews were conducted on patients who presented with cervical disc herniations. Demographic, clinical and patient reported outcome data were collected.
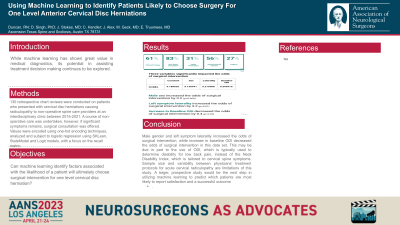
Results: Overall, 27.3% of the patients eventually choose surgical intervention with median time to surgery 17 weeks from intake. Sex was the only demographic factor to have a significant impact on surgical intervention. 38% of males underwent surgery compared to 16% of females. Body Mass Index (BMI), smoking status and comorbidities did not significantly influence the decision to have surgery, nor did any specific non-operative treatment modality (physical therapy, prescriptions, epidural steroid injections). The final optimized model yielded a test recall of 0.73. Three variables significantly impacted the odds of surgical intervention. Male sex increased the odds ratio of surgical intervention by 3.2; left symptom laterality increased the odds ratio of surgical intervention by 3.2 (p=0.01); and, interestingly, an increase in baseline Oswestry Disability Index (ODI) score decreased the odds of surgical intervention marginally by 0.4, although mean ODI scores were slightly higher in surgical patients compared to non-operative patients(30 and 28, respectively).
Conclusion : Male gender and left symptom laterality increased the odds of surgical intervention, while increase in baseline ODI decreased the odds of surgical intervention in this data set. This may be due in part to the use of ODI, which is typically used to determine disability for low back pain, instead of the Neck Disability Index, which is tailored to cervical spine symptoms.
Methods: 130 retrospective chart reviews were conducted on patients who presented with cervical disc herniations. Demographic, clinical and patient reported outcome data were collected.
Results: Overall, 27.3% of the patients eventually choose surgical intervention with median time to surgery 17 weeks from intake. Sex was the only demographic factor to have a significant impact on surgical intervention. 38% of males underwent surgery compared to 16% of females. Body Mass Index (BMI), smoking status and comorbidities did not significantly influence the decision to have surgery, nor did any specific non-operative treatment modality (physical therapy, prescriptions, epidural steroid injections). The final optimized model yielded a test recall of 0.73. Three variables significantly impacted the odds of surgical intervention. Male sex increased the odds ratio of surgical intervention by 3.2; left symptom laterality increased the odds ratio of surgical intervention by 3.2 (p=0.01); and, interestingly, an increase in baseline Oswestry Disability Index (ODI) score decreased the odds of surgical intervention marginally by 0.4, although mean ODI scores were slightly higher in surgical patients compared to non-operative patients(30 and 28, respectively).
Conclusion : Male gender and left symptom laterality increased the odds of surgical intervention, while increase in baseline ODI decreased the odds of surgical intervention in this data set. This may be due in part to the use of ODI, which is typically used to determine disability for low back pain, instead of the Neck Disability Index, which is tailored to cervical spine symptoms.
