Intraventricular Tumors: New Trends, Future Perspectives And Surgical Strategies
Intraventricular Tumors: New Trends, Future Perspectives and Surgical Strategies
Friday, April 21, 2023
Has Audio

Alessio Iacoangeli
MD
Clinica di Neurochirurgia, Ancona (Italy)
ePoster Presenter(s)
Introduction: Intraventricular tumors represent a minority in the context of brain tumors, but their treatment is particularly complex, due to their intimate relationship with eloquent neuro-vascular structures and, often, deep seated. The characteristics and localization of these tumors make them ideal candidates for mini-invasive endoscopic and\or combined micro-endo surgery, which is one of the most widely used techniques for resection of these lesions. However other surgical options must also be considered, especially for larger and third- ventricle tumors.
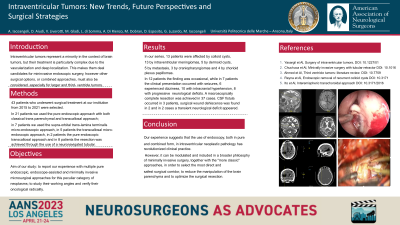
Methods: Forty-three patients with intraventricular lesions submitted to surgical treatment at our institution from 2016 to 2021 were selected. In 21 patients we used the pure endoscopic approach with classical trans parenchymal approach; in 7 patients we used the supra-orbital trans-lamina terminalis micro-endoscopic approach, in 5 patients the transcallosal micro-endoscopic approach, in 2 patients the pure endoscopic transcallosal approach and in 8 patients the resection was achieved through the use of a neuronavigated tubular approach. The following data were collected: pre and post-operative imaging, clinical outcome and complications.
Results: In our series, 13 patients were affected by colloid cysts, 13 by intraventricular meningiomas, 5 by dermoid cysts, 5 by metastasis, 3 by craniopharyngiomas and 4 by chorioid plexus papillomas. In 12 patients the finding was occasional, while in 7 patients the clinical presentation occurred with seizures, 6 experienced dizziness, 10 with intracranial hypertension, 8 with progressive neurological deficits. A macroscopically complete resection was achieved in 37 cases.
Conclusion : Our experience suggests that the use of endoscopy, both in pure and combined form, in intraventricular neoplastic pathology has revolutionized clinical practice. However, it can be modulated and included in a broader philosophy of minimally invasive surgery, together with the "more classic" approaches, in order to select the most direct and safest surgical corridor, to reduce the manipulation of the brain parenchyma and to optimize the surgical resection.
Methods: Forty-three patients with intraventricular lesions submitted to surgical treatment at our institution from 2016 to 2021 were selected. In 21 patients we used the pure endoscopic approach with classical trans parenchymal approach; in 7 patients we used the supra-orbital trans-lamina terminalis micro-endoscopic approach, in 5 patients the transcallosal micro-endoscopic approach, in 2 patients the pure endoscopic transcallosal approach and in 8 patients the resection was achieved through the use of a neuronavigated tubular approach. The following data were collected: pre and post-operative imaging, clinical outcome and complications.
Results: In our series, 13 patients were affected by colloid cysts, 13 by intraventricular meningiomas, 5 by dermoid cysts, 5 by metastasis, 3 by craniopharyngiomas and 4 by chorioid plexus papillomas. In 12 patients the finding was occasional, while in 7 patients the clinical presentation occurred with seizures, 6 experienced dizziness, 10 with intracranial hypertension, 8 with progressive neurological deficits. A macroscopically complete resection was achieved in 37 cases.
Conclusion : Our experience suggests that the use of endoscopy, both in pure and combined form, in intraventricular neoplastic pathology has revolutionized clinical practice. However, it can be modulated and included in a broader philosophy of minimally invasive surgery, together with the "more classic" approaches, in order to select the most direct and safest surgical corridor, to reduce the manipulation of the brain parenchyma and to optimize the surgical resection.
