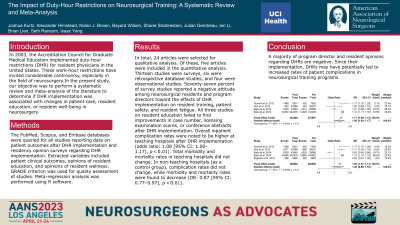
The Impact of Duty Hour Restrictions on Neurosurgical Training: a Systematic Review and Meta-Analysis.
The Impact of Duty Hour Restrictions on Neurosurgical Training: A Systematic Review and Meta-analysis
Friday, April 21, 2023
Nolan J. Brown, MBA
Junior Specialist
UC Irvine Department of Neurosurgery
Santa Clarita, California, United States
ePoster Presenter(s)
Introduction: In 2003, the Accreditation Council for Graduate Medical Education implemented duty hour restrictions (DHR) for resident physicians in the United States. These work hour restrictions have invited considerable controversy, especially in the field of neurosurgery. Our objective was to perform a systematic review and meta-analysis of the literature to determine if DHR implementation was associated with changes in patient care, resident education, or resident well-being in neurosurgery.
Methods: The PubMed, Scopus, and Embase databases were queried for all studies reporting data on patient outcomes after DHR implementation and residency opinion surveys regarding DHR implementation. Extracted variables included patient clinical outcomes, opinions of resident education, and opinions of resident wellness. GRADE criteria was used for quality assessment of studies. Meta-regression analysis was performed using R software.
Results: In total, 24 articles were selected for qualitative analysis. Of these, five articles were included in the quantitative analysis. Thirteen studies were surveys, six were retrospective database studies, and four were observational studies. Seventy-seven percent of survey studies reported a negative attitude among neurosurgical residents and program directors towards the effects of DHR implementation on resident training, patient safety, and resident fatigue. All three studies on resident education failed to find improvements in case number, licensing examination scores, or conference abstracts after DHR implementation. Overall inpatient complication rates were noted to be higher at teaching hospitals after DHR implementation (Odds Ratio: 1.08 [95% CI: 1.00-1.17], p< 0.01). Total morbidity and mortality rates in teaching hospitals did not change. In non-teaching hospitals (as a control group), complication rates did not change, while morbidity and mortality rates were found to decrease (OR: 0.87 [95% CI: 0.77-0.97], p< 0.01)
Conclusion : A majority of program director and resident opinions regarding DHRs are negative. Since their implementation, DHRs may have potentially led to increased rates of patient complications in neurosurgical training programs.
Methods: The PubMed, Scopus, and Embase databases were queried for all studies reporting data on patient outcomes after DHR implementation and residency opinion surveys regarding DHR implementation. Extracted variables included patient clinical outcomes, opinions of resident education, and opinions of resident wellness. GRADE criteria was used for quality assessment of studies. Meta-regression analysis was performed using R software.
Results: In total, 24 articles were selected for qualitative analysis. Of these, five articles were included in the quantitative analysis. Thirteen studies were surveys, six were retrospective database studies, and four were observational studies. Seventy-seven percent of survey studies reported a negative attitude among neurosurgical residents and program directors towards the effects of DHR implementation on resident training, patient safety, and resident fatigue. All three studies on resident education failed to find improvements in case number, licensing examination scores, or conference abstracts after DHR implementation. Overall inpatient complication rates were noted to be higher at teaching hospitals after DHR implementation (Odds Ratio: 1.08 [95% CI: 1.00-1.17], p< 0.01). Total morbidity and mortality rates in teaching hospitals did not change. In non-teaching hospitals (as a control group), complication rates did not change, while morbidity and mortality rates were found to decrease (OR: 0.87 [95% CI: 0.77-0.97], p< 0.01)
Conclusion : A majority of program director and resident opinions regarding DHRs are negative. Since their implementation, DHRs may have potentially led to increased rates of patient complications in neurosurgical training programs.
