Pain Interference Influence on Postoperative Clinical Trajectory in Patients Undergoing Lumbar Decompression
Friday, April 21, 2023

James W. Nie, BS (he/him/his)
Medical Student
University of Illinois College of Medicine
Chicago, Illinois, United States
ePoster Presenter(s)
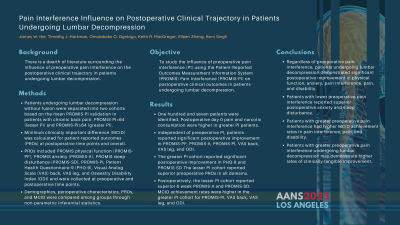
Introduction: We aim to study the influence of preoperative pain interference (PI) using the Patient-Reported Outcomes Measurement Information System (PROMIS) Pain Interference (PROMIS-PI) on postoperative clinical outcomes in patients undergoing lumbar decompression.
Methods: Patients undergoing lumbar decompression without fusion were separated into two cohorts based on the mean PROMIS-PI validation in patients with chronic back pain: PROMIS-PI < 64 (lesser PI) and PROMIS-PI≥64 (greater PI). Minimum clinically important difference (MCID) was calculated for patient-reported outcomes (PROs) at postoperative time points and overall. PROs included PROMIS physical function (PROMIS-PF), PROMIS anxiety (PROMIS-A), PROMIS sleep disturbance (PROMIS-SD), PROMIS-PI, Patient Health Questionnaire-9 (PHQ-9), Visual Analog Scale (VAS) back, VAS leg, and Oswestry Disability Index (ODI) and were collected at preoperative and postoperative time points. Demographics, perioperative characteristics, PROs, and MCID were compared among groups through non-parametric inferential statistics.
Results: One hundred and seven patients were identified. Postoperative day 0 pain and narcotic consumption were higher in greater PI patients (p=0.009). Independent of preoperative PI, patients reported significant postoperative improvement in PROMIS-PF, PROMIS-A, PROMIS-PI, VAS back, VAS leg, and ODI (p≤0.047,all). The greater PI cohort reported significant postoperative improvement in PHQ-9 and PROMIS-SD. The lesser PI cohort reported superior preoperative PROs in all domains (p≤0.001,all). Postoperatively, the lesser PI cohort reported superior 6-week PROMIS-A and PROMIS-SD (p≤0.016, both). MCID achievement rates were higher in the greater PI cohort for PROMIS-PI, VAS back, VAS leg, and ODI (p≤0.027,all).
Conclusion : Regardless of preoperative pain interference, patients undergoing lumbar decompression demonstrated significant postoperative improvement in physical function, anxiety, pain interference, pain, and disability. Patients with lower preoperative pain interference reported superior postoperative anxiety and sleep disturbance. Patients with greater preoperative pain interference had higher MCID achievement rates in pain interference, pain, and disability. Patients with greater preoperative pain interference undergoing lumbar decompression may demonstrate higher rates of clinically tangible improvement.
Methods: Patients undergoing lumbar decompression without fusion were separated into two cohorts based on the mean PROMIS-PI validation in patients with chronic back pain: PROMIS-PI < 64 (lesser PI) and PROMIS-PI≥64 (greater PI). Minimum clinically important difference (MCID) was calculated for patient-reported outcomes (PROs) at postoperative time points and overall. PROs included PROMIS physical function (PROMIS-PF), PROMIS anxiety (PROMIS-A), PROMIS sleep disturbance (PROMIS-SD), PROMIS-PI, Patient Health Questionnaire-9 (PHQ-9), Visual Analog Scale (VAS) back, VAS leg, and Oswestry Disability Index (ODI) and were collected at preoperative and postoperative time points. Demographics, perioperative characteristics, PROs, and MCID were compared among groups through non-parametric inferential statistics.
Results: One hundred and seven patients were identified. Postoperative day 0 pain and narcotic consumption were higher in greater PI patients (p=0.009). Independent of preoperative PI, patients reported significant postoperative improvement in PROMIS-PF, PROMIS-A, PROMIS-PI, VAS back, VAS leg, and ODI (p≤0.047,all). The greater PI cohort reported significant postoperative improvement in PHQ-9 and PROMIS-SD. The lesser PI cohort reported superior preoperative PROs in all domains (p≤0.001,all). Postoperatively, the lesser PI cohort reported superior 6-week PROMIS-A and PROMIS-SD (p≤0.016, both). MCID achievement rates were higher in the greater PI cohort for PROMIS-PI, VAS back, VAS leg, and ODI (p≤0.027,all).
Conclusion : Regardless of preoperative pain interference, patients undergoing lumbar decompression demonstrated significant postoperative improvement in physical function, anxiety, pain interference, pain, and disability. Patients with lower preoperative pain interference reported superior postoperative anxiety and sleep disturbance. Patients with greater preoperative pain interference had higher MCID achievement rates in pain interference, pain, and disability. Patients with greater preoperative pain interference undergoing lumbar decompression may demonstrate higher rates of clinically tangible improvement.
